Lumbar Spinal
Stenosis
Dr.
Rami Rustum
 Lumbar spine stenosis is the
most common cause of lower back pain in
middle aged and elderly people. Lumbar spine stenosis is the
most common cause of lower back pain in
middle aged and elderly people.
The lumbar spine canal is formed by
vertebrae, ligaments and discs. The canal
hosts the nerves allowing them to emerge
to both sides of the spine through
special openings called foramen.
As we age, more calcium is randomly
deposited in these “openings”,
ligaments and discs resulting in stiffer
and smaller spinal canal as shown in the
graph below.
As the lumbar spinal canal narrows, the
nerves that go through it are squeezed.
This squeezing may cause back pain, and
leg pain and weakness.
The causes for having calcified spinal
canal may vary but it is believed to be
as a result of arthritis, previous falls,
accidents, and wear and tear on the
spine’s bones and joints.
It is important here to point out that
spinal stenosis can affect any part of
the spine including the cervical region
(neck) however the problem is seen in the
lumbar spine in 75-80% of all cases.
What are the symptoms of lumbar spinal
stenosis?
It is clear now that people have
different pain tolerances and experience
pain differently. Based on that, people
present to the pain clinic with a variety
of complaints. However, the most common
ones are: Lower back ache, lower back
pain radiating to the legs upon walking
or standing, leg cramps, and leg
numbness.
Symptoms usually get better with resting,
bending slightly forward or lying in
fetal position on the side with the knees
brought up to the chest. It’s
thought that these positions
“open” the lumbar canal and
take the pressure off the nerves that go
to the legs.
In advanced stages, difficulty walking
can occur, as well as problems with bowel
and bladder control.
How is lumbar spinal stenosis diagnosed?
As with any disease, the patient’s
history and physical exam are the
cornerstone of the diagnosis!
 During the medical history,
the patient will be asked questions
regarding symptoms including: How long
they have been present? What make it
better or worse? What prior treatment the
patient has had? What other medical
conditions they have? These questions can
help the doctor distinguish lumbar spinal
stenosis from other disorders. During the medical history,
the patient will be asked questions
regarding symptoms including: How long
they have been present? What make it
better or worse? What prior treatment the
patient has had? What other medical
conditions they have? These questions can
help the doctor distinguish lumbar spinal
stenosis from other disorders.
Plain x-rays of the back is usually
ordered. The x-rays can show the doctor
various signs associated with spinal
stenosis including loss of the normal
intervertebral disc height, bone spurs
(osteophytes), and spinal instability
(abnormal motion between the vertebrae).
The ultimate diagnosis of lumbar spinal
stenosis is made with an MRI (magnetic
resonance imagining) scan or CT (computed
tomography) scan. These are more advanced
tests that show the nerves in the lower
back and can show if they are being
compressed from lumbar spinal stenosis.
What is the treatment for lumbar spinal
stenosis?
In most cases the treatment for lumbar
spinal stenosis begins with conservative
(non-surgical) treatment. This can
include medications to reduce
inflammation, short courses of oral
cortisone medication, and pain
medications. There are also several
medications directed specifically at
nerve pain that are helpful in lumbar
spinal stenosis, including gabapentin
(Neurontin) and pregabalin (Lyrica). I
find the adding of muscle relaxant like
Baclofen or Flexeril is also very
helpful.
Physical therapy can help in some
cases especially with the use of TENS
unit treatment.
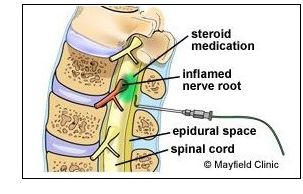
Cortisone (steroid) injections in the
lumbar spine can also reduce the symptoms
by decreasing inflammation and swelling
around the nerve tissue.
An epidural steroid injection is
generally successful in relieving pain in
approximately 50% of patients. If a
patient does not experience any back pain
or leg pain relief from the first
epidural injection, further injections
will probably not be beneficial. However,
if there is some improvement in back pain
or leg pain, one to two additional
epidural steroid injections may be
recommended. These can be repeated up to
three times per year. 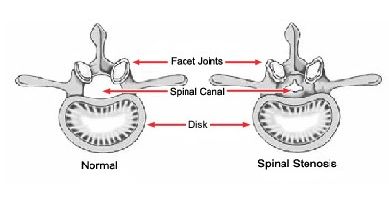
As with any invasive medical procedures,
there are potential risks associated with
lumbar epidural steroid injections.
Generally, however, there are few risks
associated with epidural steroid
injections and they tend to be rare.
Risks may include:
• Infection. Minor infections occur
in 1% to 2% of all injections. Severe
infections are rare, occurring in 0.1% to
0.01% of injections.
• Bleeding. Bleeding is a rare
complication and is more common for
patients with underlying bleeding
disorders or taking blood thinners.
• Nerve damage. While extremely
rare, nerve damage can occur from direct
trauma from the needle, or secondarily,
from infection or bleeding.
• Dural puncture (“wet
tap”). A dural puncture occurs in
0.5% of injections. It may cause a
post-dural puncture headache (also called
a spinal headache) that usually gets
better within a few days. Although rare,
a blood patch may be necessary to
alleviate the headache.
Paralysis is not a risk since there is no
spinal cord in the region of the epidural
steroid injection.
In addition to risks from the injection,
there are also potential risks and side
effects from the steroid medication.
These side effects from an epidural
steroid injection tend to be rare. Side
effects from steroids are more common
when taken daily for several months.
Risks and side effects may include:
• High blood sugar
• Stomach ulcers
• Fluid retention and weight gain
• Cataracts
• Facial flushing
• Metallic taste in the mouth
• Increased appetite Lumbar
epidural steroid injections should not be
performed on patients who have a local or
systemic bacterial infection, are
pregnant, or have bleeding problems.
Epidural steroid injections should also
not be performed on patients whose pain
is from a tumor or infection, and if
suspected, an MRI scan should be done
prior to the injection to rule out these
conditions.
Surgical Treatment
In general, surgery is only considered as
a last resort if all attempts at
nonsurgical therapies are unsuccessful,
and if the overall potential benefits of
surgery are greater than the potential
risks. Surgery may be recommended on an
urgent basis if a patient has severe
weakness or loss of bowel and bladder
control.
If surgery is ultimately necessary, the
surgery most commonly performed to
decompress the spinal canal is called a
lumbar laminectomy.
Is lumbar spinal stenosis preventable?
Unfortunately, the degenerative changes
responsible for lumbar spinal stenosis
can occur as part of the normal ageing
process. There is little that can be done
to prevent lumbar spinal stenosis.
Remember: this is what you may pay for
too many birthdays!!!!
>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
All pictures and
material are
(C) copyright, Valley Patriot, Inc., 2008
|